For women undergoing in vitro fertilisation (IVF) followed by a frozen embryo transfer, using a natural ovulation cycle is just as effective as hormone-based preparation of the uterus—and comes with fewer risks to both mother and baby. A large-scale, randomised trial involving over 4,300 women confirms this, potentially shifting standard practices in fertility treatment.
The Rise of Frozen Embryo Transfers
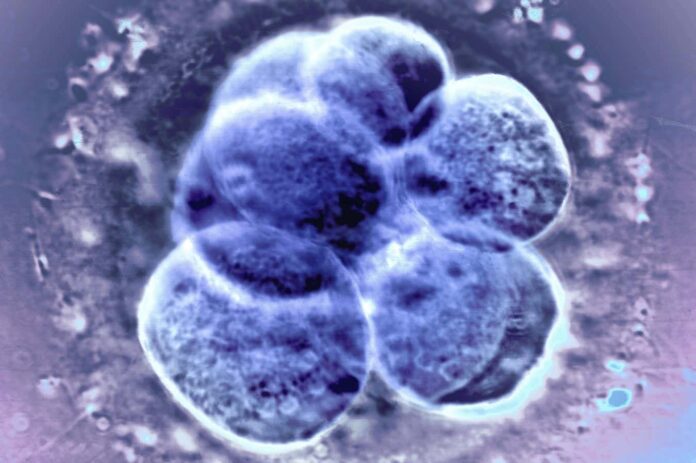
In recent years, frozen embryo transfers (FETs) have become increasingly common, now accounting for the majority of embryo transfers globally. This is partly because freezing embryos allows for better timing: a frozen embryo can be transferred to the uterus when conditions are optimal for implantation. But preparing the uterus for this transfer requires either hormone treatment or reliance on the body’s natural cycle.
For years, it was unclear which approach was superior. Both have been assumed to provide comparable success rates, yet neither had been definitively proven by large-scale research.
The Trial Findings: Similar Success, Lower Complications
Researchers at Shandong University in China conducted a trial with 4,376 women planning FETs. Half used medicated cycles (hormones to prepare the uterus), while the other half relied on their natural menstrual cycles. Live birth rates were nearly identical: 41.6% for the natural cycle group versus 40.6% for the medicated group.
However, the study revealed significant differences in maternal health. Women using their natural cycles had notably lower rates of:
- Pre-eclampsia : A dangerous pregnancy complication involving high blood pressure.
- Early pregnancy loss : Miscarriage in the first trimester.
- Placental accreta spectrum : A condition where the placenta doesn’t detach easily after birth, potentially leading to severe bleeding.
- Caesarean sections and postpartum hemorrhage.
These complications don’t just impact the current pregnancy but can lead to long-term health problems for the mother.
Why Natural Cycles May Be Safer
Experts suggest the presence of a corpus luteum —a temporary structure formed in the ovary after ovulation—may be key. This structure produces hormones that prepare the uterus for pregnancy and may play a protective role against pre-eclampsia. While more research is needed to confirm this mechanism, the study strongly suggests natural cycles offer distinct advantages.
“This is the randomised-controlled trial we have been waiting for,” says William Buckett of McGill University, underscoring the study’s importance.
Future Research: Identifying Biomarkers
The research team is now analyzing blood samples collected during the trial to identify biomarkers that may explain the observed differences in pregnancy complications. This could lead to more targeted interventions and even better outcomes for women undergoing FET.
In conclusion, this study provides strong evidence that natural ovulation is a safe, effective, and potentially healthier option for preparing the uterus for frozen embryo transfers, challenging conventional wisdom and opening the door to more informed fertility treatment decisions.