A new cancer vaccine has demonstrated encouraging results in laboratory studies, showing the potential to treat HPV-related throat cancers. The research, published in Science Advances, highlights a unique approach to vaccine design that could improve effectiveness beyond existing treatments and offer insights into building better vaccines for other diseases.
The Rising Threat of HPV-Driven Cancers
Human papillomavirus (HPV) is widely known as the cause of most cervical cancers, but it’s also responsible for a significant and growing number of other cancers, including oropharyngeal cancer (throat cancer). In the United States, roughly 70% of these throat cancers are linked to HPV, with strain 16 being the primary culprit. While the Gardasil 9 vaccine prevents HPV infection, current treatment options for those already diagnosed with HPV-related tumors remain limited to surgery, radiation, and chemotherapy.
This is where the new vaccine steps in. The goal isn’t prevention, but treatment —to enhance the body’s immune response against existing tumors and reduce the risk of recurrence.
A Smarter Vaccine Design: The Power of Structure
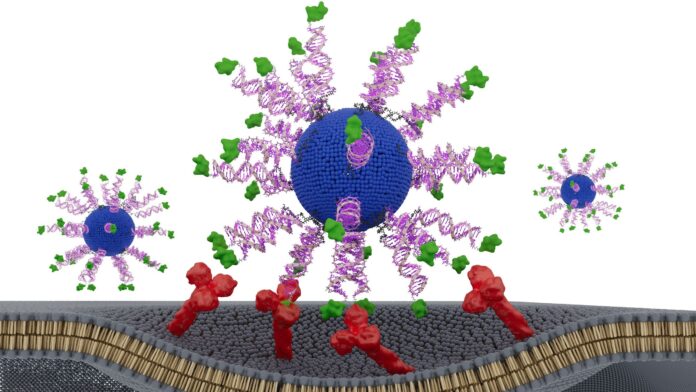
The breakthrough isn’t just about what is in the vaccine, but how it’s arranged. Researchers engineered a vaccine using spherical nucleic acids (SNAs) – globe-shaped DNA particles that deliver antigens (the target proteins) directly to immune cells. This differs from traditional linear DNA-based vaccines, which are less effective at entering cells.
The team tested three SNA designs, varying only in how the HPV protein fragment was attached. The key finding: positioning the fragment via its N-terminus (one end of its structure) triggered the strongest immune response. This led to up to eight times more interferon-gamma production —a critical signal for antitumor activity—making killer T cells far more effective at destroying cancer cells.
Lab and Animal Study Results: A Clear Advantage
In laboratory tests on HPV-positive head and neck cancer cells, the optimized vaccine slowed tumor growth significantly in mice. Critically, when tested on real tumor samples from patients, it killed two to three times more cancer cells compared to other designs. The effect wasn’t due to stronger ingredients, but to smarter presentation.
As Dr. Jochen Lorch, medical oncology director at Northwestern Medicine, put it, “The immune system is sensitive to the geometry of molecules. By optimizing how we attach the antigen to the SNA, the immune cells processed it more efficiently.”
What This Means for Future Cancer Therapies
While human trials are still needed, this research suggests that optimizing vaccine structure, not just content, could unlock far more effective cancer treatments. According to Dr. Ezra Cohen of UC San Diego Health, if proven successful in humans, this vaccine could be combined with existing therapies to eliminate disease and prevent recurrence.
The implications extend beyond HPV. Inventor Chad Mirkin believes this approach could revitalize previously unsuccessful vaccine candidates simply by restructuring their components.
“We may have passed up perfectly acceptable vaccine components simply because they were in the wrong configurations. We can go back to those and restructure and transform them into potent medicines.”
This discovery underscores the importance of precision in vaccine development, suggesting that even minor structural changes can yield dramatically improved results.